INFECTION PREVENTION & CONTROL
After every crisis nothing remains the same. This will be true even when the current emergency will be over. Clinics, dental practices, GPs will therefore inevitably have to learn to manage all patients as possible asymptomatic or paucisymptomatic carriers as also indicated by Health Ministers worldwide:
- Use robust infection prevention and control procedures in line with government advice.
- Consideration should be given to both patient group and the type of treatment undertaken (i.e. increased risk associated with aerosol generating procedures means there are additional PPE and decontamination requirements).
- Additional physical and temporal separation measures should be taken for groups at increased risk where possible, allowing maximum time for air clearance/ventilation overnight(BDA).
OZONE IS THE ANSWER TO COMPLY WITH NEW GUIDLINES WHILST MANTAINING HIGH OPERATIONAL STANDARS AND EFFICIENCY
Moreover, recent evidence has shown how Coronaviruses (SARS-CoV-2 too) have the ability to circulate and persist in the air and not only through droplets. This has an enormous impact on the clinic’s air quality, especially at the end of a working day when it will result poor.
- the greater the number of air changes per hour(ventilation rate), the sooner any aerosol will be cleared.
- Where feasible, environmental decontamination should be performed: A minimum of 20 minutes, that is 2 air changes, in clinical settings where the majority of these procedures occur is considered pragmatic(UK GOV Transmission characteristics and principles of infection prevention and control).
IS OZONE SAFE?
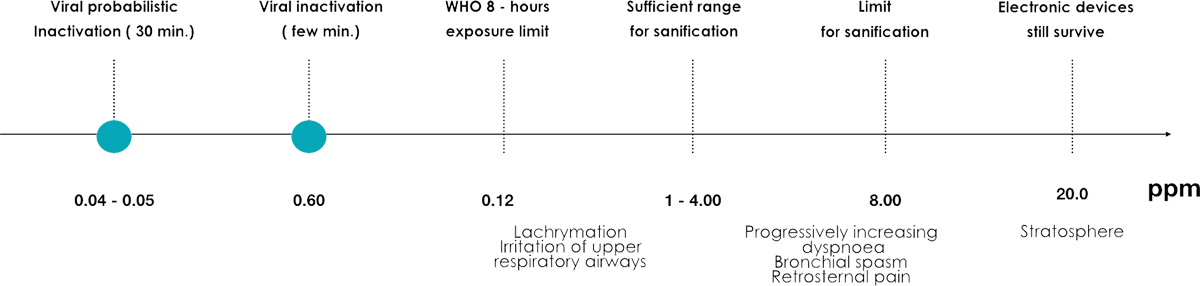
Low ozone concentration, given the absence of danger to the respiratory tract, can be used during operational activity, so as to contain microbial contamination and viruses in activation.
Higher concentration, which can be toxic, can instead be used for a profound sanitation of the environment during the hours of suspension of the operating activity or between patients.