OUR VISION
Living and working in a sane and safe environment is of paramount importance and today, more than ever, a priority. Finding a way to do it sustainably and effectively, according to our protocols and procedures is the challenge and our mission.
WHY TO CHOOSE OZONE-BASED SANITIZATION?
Total surface and air sanitization with conventional procedures is not technically possible nor economically sustainable. The use of an active gas that can spread to all environments constitutes a formidable solution.
- Guarantees elimination of 99.9% viruses, bacteria, molds and yeasts
- Its highly oxidizing and sanitizing power reaches all surfaces even the most hidden ones (differently from UV radiation and HEPA filter)
- When produced with quality devices, ozone is completely safe and there are no contraindications
- Sanitization happens in short time fitting your clinical protocols
- Its cost-effectiveness compared to traditional chemicals and reduces staff related costs (no labour nor ordinary maintenance)
- Environment friendly: No organic nor inorganic harmful residues are left after disinfection (being unstable, Ozone is readily converted back to oxygen)
- Use robust infection prevention and control procedures in line with government advice
- Consideration should be given to both patient group and the type of treatment undertaken (i.e. increased risk associated with aerosol generating procedures means there are additional PPE and decontamination requirements)
- Additional physical and temporal separation measures should be taken for groups at increased risk where possible, allowing maximum time for air clearance/ventilation overnight (NHS)
Moreover, recent evidence has shown how Corona viruses (SARS-CoV-2 too) have the ability to circulate and persist in the air and not only through droplets. This has an enormous impact on the clinic’s air quality, especially at the end of a working day when it will result poor
- The rate of clearance of aerosols in an enclosed space is dependent on the extent of any mechanical or natural ventilation – the greater the number of air changes per hour (ventilation rate), the sooner any aerosol will be cleared
- Where feasible, environmental decontamination should be performed: A minimum of 20 minutes, that is 2 air changes, in clinical settings where the majority of these procedures occur is considered pragmatic (NHS Transmission characteristics and principles of infection prevention and control)
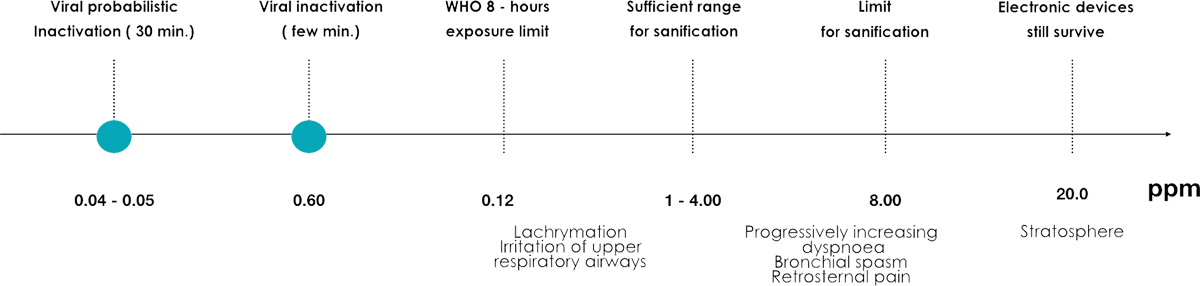
Low ozone concentration, given the absence of danger to the respiratory tract, can be used during operational activity, so as to contain microbial contamination and viruses.
Higher concentration, which can be toxic, can instead be used for a profound sanitation of the environment during the hours of suspension of the operating activity or between patients
INACTIVATION OF VIRUSES, BACTERIA, MOLDS, YEASTS AND INSECTS
The antipathogenic effects of ozone have been substantiated for several decades (its killing action upon bacteria, viruses, fungi, and in many species of protozoa).
The effectiveness of disinfection depends on the susceptibility of the target organisms, the contact time, and the concentration of the ozone as indicated in the chart :
| ORGANISM | CONCENTRATION | EXPOSITION TIME |
|---|---|---|
| Virus (Polio virus type-1, Human Rotavirus, Flu, Enteric virus) |
0.2 ppm – 4.1 ppm | < 20 minutes |
| Bacteria (E. Coli, Legionella, Mycobacterium, Fecal Streptococcus) |
0.23 ppm – 2.2 ppm | < 20 minutes |
| Molds (Aspergillus Niger, vari ceppi di Penicillum, Cladosporium) |
2 ppm | 60 minutes |
| Yeasts (Candida Parapsilosis, Candida Tropicalis) |
0.02 ppm – 0.26 ppm | < 1,67 minutes |
| Insects (Acarus Siro, TyrophagusCasei, TyrophagusPutrescientiae) |
1.5 – 2 ppm | 30 minutes |